Evolving Healthcare Hiring Trends: What Today’s Market Is Telling Us
The healthcare labor market is shifting rapidly. As hospitals and clinics compete to recruit qualified providers, several data-backed trends are emerging—around flexibility, burnout, locum tenens growth, and technology adoption. If you’re hiring NPs, APPs, or physicians, aligning with these trends will help you attract and retain top-tier talent.
-
Flexible Scheduling Is Now Expected
A 2024 report from the Massachusetts Center for Health Information and Analysis (CHIA) highlights that inflexible scheduling and high burnout are among the top concerns in ambulatory care and community health settings. Similarly, recent HHS research underscores the role of flexible work models in stabilizing healthcare staffing.
Why it matters:
Clinicians are seeking part-time, per diem, and remote-friendly options. Organizations offering more control over scheduling are seeing improved recruitment and retention rates.
-
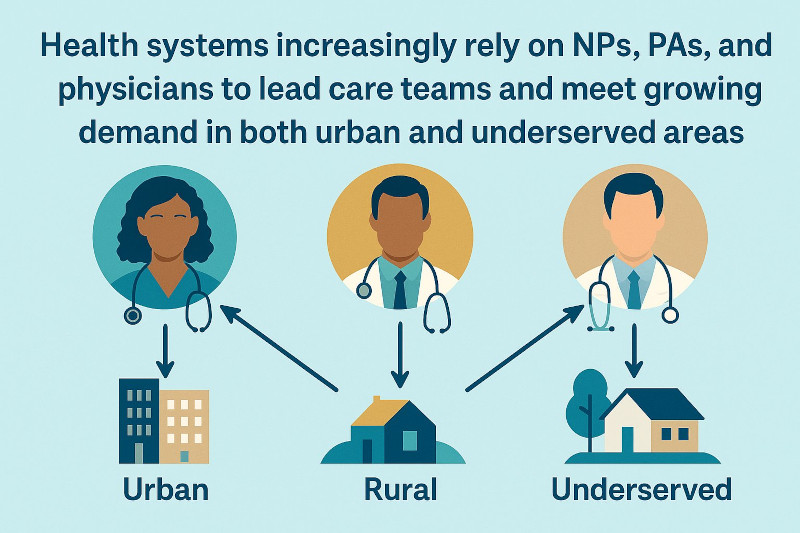
Demand for Advanced Practice Providers Continues to Climb
Data from the Health Resources and Services Administration (HRSA) project shortages in multiple advanced provider roles, including primary care physicians, psychiatrists, and pharmacists, through 2037. On the state level, Texas DSHS projects a 9,600-FTE primary care physician shortfall by 2036.
Why it matters:
Hiring isn’t just about nurses. Health systems increasingly rely on NPs, PAs, and physicians to lead care teams and meet growing demand in both urban and underserved areas.
-
Locum Tenens Is No Longer a Niche Strategy
A Precedence Research market report estimates that the U.S. locum tenens sector—valued at $3.5 billion in 2023—will reach nearly $8 billion by 2034. Meanwhile, Staffing Industry Analysts data confirms year-over-year double-digit growth in locum coverage for both generalist and specialty providers.
Why it matters:
More clinicians are choosing contract-based roles for better flexibility and lifestyle control. Offering locum or temp-to-perm positions allows you to stay agile in the face of coverage gaps and fluctuating demand.
-
Technology Is Accelerating Hiring Efficiency
According to ASPE at HHS, digital tools like mobile scheduling, same-day pay, and credentialing automation are critical to the future of healthcare staffing. Providers—especially younger clinicians—now expect tech-enabled onboarding, e-pay, and streamlined workflows.
Why it matters:
Outdated systems lead to lost candidates. Adopting digital platforms for recruiting and placement is no longer optional—it’s a core part of competitive hiring.
-
Burnout Is Reshaping How We Hire
Both the CHIA report and ASPE brief identify burnout and staff shortages as structural threats to care access. These reports tie workforce gaps to delayed treatments and higher patient risk in multiple specialties.
Why it matters:
Relying solely on permanent hires can lead to burnout and turnover. A balanced staffing strategy—with supplemental support like locums—can stabilize teams and maintain patient care standards.
How Momentum Healthcare Staffing Aligns with These Trends
At Momentum Healthcare Staffing, we recruit for the world healthcare is becoming—not the one it used to be. Our placements support:
- Flexible staffing models – Including per diem, telehealth, locum, and full-time placements
- In-demand specialties – Like urgent care, geriatrics, psychiatry, and primary care
- Technology-driven recruitment – With efficient onboarding, scheduling, and credentialing
- Retention and resilience – Helping you reduce burnout and maintain quality of care
Whether you’re a facility trying to reduce turnover or a system scaling services, we’ll help you find clinicians who are ready for what’s next.
Let’s Build Your Ideal Care Team
📞 Call us at (877) 558‑3782 or visit https://momentumhcs.com/contact/ to get started. Our team can help you hire the providers that today’s healthcare environment demands.




















Recent Comments